Salesforce Health Cloud Implementation Guide 2025
MarketsandMarkets forecasts that the global healthcare cloud computing market is expected to grow from $53.8 billion in 2024 to $120.6 billion by 2029, representing a compound annual growth rate (CAGR) of 17.5%. This trend is due to the adoption of cloud-based solutions across the healthcare industry, which increases storage space and compute power, making it more cost-effective.
According to a HIMSS survey, healthcare organizations juggle over 46 different systems on average, leading to inefficient processes and data silos. Meanwhile, 80% of patients report difficulties navigating their care journey, and 77% are open to virtual visits for non-emergency needs.¹ These trends make it clear: to deliver seamless, patient-first care, healthcare organizations need more than traditional EMRs. They need intelligent platforms like Salesforce Health Cloud.
The Salesforce Health Cloud is leading this change, offering integrated services to improve the care delivery process. This blog delves into the specifics of implementing the Salesforce Health Cloud, looking at its benefits and features and comparing them with healthcare regulations.
What is Salesforce Health Cloud?
Salesforce Health Cloud is a cloud-native CRM platform purpose-built for the healthcare and life sciences industry. Unlike electronic medical records (EMRs) that focus narrowly on clinical documentation, Health Cloud creates a 360-degree patient view by unifying demographic, clinical, and behavioral data in one platform. It integrates with EHRs, telehealth systems, wearables, and billing platforms—so care teams have the full patient story at their fingertips.
Since its launch in 2016, Health Cloud has evolved into a core component of Salesforce Customer 360 for Health, combining Data Cloud, AI (Einstein), and Flow Automation to drive smarter care. Key innovations like MuleSoft Direct for Health Cloud, native telehealth integrations, and Einstein Copilot for care management make it a flexible yet powerful solution for modern healthcare.
“Artificial super intelligence will evolve into Super Wisdom and contribute to the happiness of all humanity.”
– Masayoshi Son, CEO of SoftBank
Key Features and Benefits of Salesforce Health Cloud
1. Unified Patient Data (Patient 360)
Salesforce Health Cloud breaks down data silos by consolidating patient information across EHRs, claims, devices, and social determinants of health (SDoH). The Health Timeline feature visualizes every encounter, medication change, lab result, and clinical note, enabling providers to make informed decisions in real time.
2. Care Coordination and Personalization
Health Cloud enables the creation of personalized care plans, assigning goals, tasks, and milestones to each patient. With secure messaging, task automation, and cross-team collaboration, care managers and providers can stay aligned across the patient’s journey.
Example: Automated follow-ups for post-discharge patients can be triggered using Salesforce Flows, improving recovery and reducing readmissions.
3. Omnichannel Patient Engagement
Health Cloud supports SMS, email, patient portals, and video calls. Embedded two-way video visits via Salesforce SOS enhance virtual care experiences, allowing providers to update patient records in real time while engaging patients remotely.
4. Privacy, Security, and Compliance
Built with healthcare in mind, Health Cloud is HIPAA-compliant out of the box. Features include:
Role-based access
Multi-factor authentication (MFA)
End-to-end encryption (at rest and in transit)
These capabilities enable organizations to safeguard Protected Health Information (PHI) while still leveraging it to improve care delivery.
5. AI and Predictive Analytics
Einstein AI enables:
Risk stratification for chronic conditions
Proactive intervention alerts
Natural language care plan generation using Einstein Copilot
Salesforce’s integration with Tableau and Data Cloud further allows organizations to track patient outcomes, segment populations, and visualize KPIs across departments.
6. Integration and Interoperability
With FHIR-based APIs and MuleSoft Direct, Health Cloud integrates seamlessly with:
Major EHRs (e.g. Epic, Cerner)
Telehealth platforms
Remote monitoring devices
Insurance and billing systems
This makes Health Cloud the unifying layer across legacy and modern systems.
Related Read – Salesforce CRM Implementation With AI – The Ultimate Guide
Salesforce Health Cloud Implementation Steps
1. Define Business Objectives
Start with clear goals:
Reduce readmissions?
Improve care coordination?
Enhance patient engagement?
Align your objectives with broader organizational strategies like digital transformation or value-based care.
2. Build a Cross-Functional Team
Include:
Executive sponsor (e.g. CIO or VP of Clinical Ops)
Salesforce Administrator and Health Cloud consultants
Clinical SMEs (nurses, care managers)
IT integration experts
Project managers and adoption champions
3. Assess Current Data Landscape
Conduct a full audit of existing patient data—EHRs, spreadsheets, third-party CRMs. Clean up duplicate records and standardize field mappings to fit Health Cloud’s data model.
4. Configure & Customize the Platform
Configure:
Patient objects, care plans, and tasks
Sharing rules and data visibility
Custom dashboards and Lightning pages
Use “clicks not code” whenever possible, leveraging Salesforce Flows and Process Builder. Avoid over-customization to ensure future compatibility.
5. Integrate Early and Smartly
Prioritize EHR integrations using FHIR standards. Enable bidirectional data sync (e.g., new notes in Health Cloud updating the EHR). Don’t overlook pharmacy, billing, or telehealth system integrations—these add tremendous value.
6. Change Management and Training
Even the most advanced platforms fail without user adoption. Change management is not an afterthought—it’s a core success factor.
Best practices:
Develop role-specific training: Use hands-on sandbox demos tailored to actual workflows (e.g. “How to create a Care Plan task”).
Designate super-users: Empower departmental champions to train peers and gather feedback.
Communicate value: Show how Health Cloud simplifies daily work, like reducing time spent on scheduling or enabling faster patient follow-ups.
Gather feedback: Run regular listening sessions to uncover adoption blockers and opportunities for improvement.
7. Testing and Quality Assurance
Before go-live, thoroughly test:
System configuration: Ensure security roles, record access, and data model integrity.
Integration logic: Validate all APIs and FHIR connections are syncing bi-directionally with no data loss.
User Acceptance Testing (UAT): Simulate real-world use cases across departments—admissions, care transitions, billing—to ensure a smooth handoff.
8. Go-Live and Deployment
Organizations can choose either a phased rollout (e.g., pilot in one clinic) or a big bang launch. Phased approaches typically offer smoother transitions and room to iterate.
On go-live:
Set up on-site or virtual support teams.
Reiterate benefits to staff to boost morale and confidence.
Track early KPIs to catch any red flags quickly.
9. Monitoring, Support, and Optimization
Health Cloud is not a “set and forget” system.
Monitor adoption through usage metrics and feedback surveys.
Track performance using Tableau dashboards and login metrics.
Support users with a responsive help desk and documentation.
Iterate regularly—incorporate new Salesforce releases, address bottlenecks, and refine automations based on real-world usage.
10. Continuous Improvement
Adopt new features like Einstein Copilot, Tableau Pulse, or Advanced Therapy Management.
Conduct quarterly stakeholder reviews to realign system use with evolving business goals.
Optimize data quality and enrich records with new data sources over time.
Overcoming Implementation Challenges
Healthcare implementations are complex. Here’s how to anticipate and avoid common Health Cloud pitfalls:
| Challenge | Solution |
| Replicating inefficient workflows | Rethink and redesign processes, don’t just digitize legacy tasks |
| Poor change management | Engage users early, train thoroughly, and highlight time-saving benefits |
| Data quality and migration issues | Allocate time for data cleansing and use experienced migration partners |
| Over-customization | Stick to Salesforce best practices; prioritize “clicks over code” |
| Integration delays | Use FHIR and pre-built MuleSoft connectors for faster interoperability |
| No long-term roadmap | Define a phased strategy aligned to broader transformation goals |
Also Read – Salesforce CPQ Implementation Guide
Integration Strategy: A Unified Architecture
Health Cloud’s power lies in connecting disparate systems:
| Integration Point | Purpose |
| EHR Systems (e.g. Epic) | Sync diagnosis, labs, notes into patient timeline |
| Data Cloud (CDP) | Aggregate SDoH, device, and claim data into a single source of truth |
| Telehealth | Embed video visits, update care plans in real time |
| Remote Monitoring (IoT) | Trigger alerts from home-based readings (e.g. BP, glucose monitors) |
| Billing & Claims Systems | Automate eligibility checks and prior authorization workflows |
As Amit Khanna, SVP at Salesforce Health, aptly states:
“The future of care is proactive, personalized, and connected. Health Cloud is the platform to build that future.”
Conclusion
With the help of Salesforce Health Cloud implementation, healthcare organizations can transform themselves into more efficient units towards better patient care in the challenging scenario of modern healthcare. Healthcare providers can integrate this powerful tool with current technologies to make patient care practices more personalized, insightful, and secure.
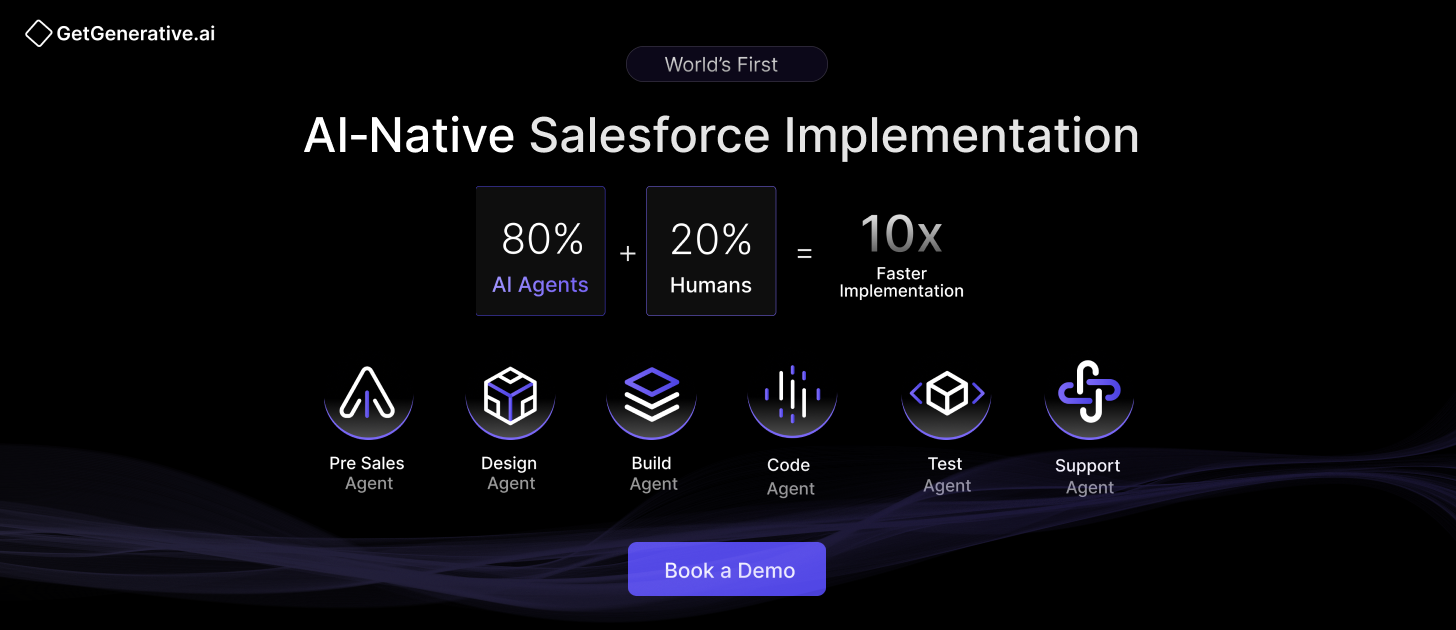
If you’re looking for help with Salesforce implementation, explore our AI Salesforce Consulting Services for expert guidance tailored to your business.
Frequently Asked Questions (FAQs)
1. What makes Salesforce Health Cloud different from other medical CRM systems?
Salesforce Health Cloud is specifically designed for healthcare, integrating deeply with clinical data and supporting compliance with healthcare regulations, which sets it apart from generic CRM systems.
2. Can Salesforce Health Cloud be integrated with any EHR system?
Yes, Salesforce Health Cloud can be integrated with various EHR systems through its interoperability capabilities, ensuring that patient data flows seamlessly between systems.
3. What is the typical implementation timeframe for Salesforce Health Cloud?
The implementation timeframe can vary based on the scale of the operation and specific needs but generally ranges from a few months to a year.
4. How is patient data secured in Salesforce Health Cloud?
Patient data is secured through encryption, both in transit and at rest, comprehensive access controls, and regular security audits.
5. Can Salesforce Health Cloud handle large volumes of patients?
Yes, it is built on the scalable Salesforce platform, which is capable of handling large volumes of data and patients efficiently.
6. How does Salesforce Health Cloud Handle Data Privacy?
The most significant concern in healthcare is data privacy. Salesforce Health Cloud is, therefore, equipped with a robust security layer to protect sensitive patient information. For instance, it uses some best-of-breed data encryption, verifies access through authentication of who’s trying to access an account, and maintains strict limits on access.
7. Is Salesforce Health Cloud Compliant with International Healthcare Regulations?
- HIPAA (Health Insurance Portability and Accountability Act) ensures the confidentiality and security of healthcare information.
- GDPR (General Data Protection Regulation) in Europe addresses data protection and privacy in the European Union and the European Economic Area.
- Other regional regulations depend on the geographical area of operation.
These levels of compliance help healthcare organizations maintain standards and avoid data breaches and penalties for non-compliance.